A. Introduction
Welcome to the Internal Medicine COVID-19 Team. First, we want to thank you for your service in caring for these sick patients during these unprecedented and uncertain times. Additionally, we want to thank you for the sacrifice you made by being on the front lines during this pandemic. Although, we hope the public health initiatives will curtail the spread of this disease to avoid overwhelming levels, we understand the paramount importance of preparation for mass casualty and disaster events. In this light, we have provided a survival guide with important information on COVID-19 as well as the evaluation, admission, management, and discharge of COVID-19 patients as it pertains to Naval Medical Center Portsmouth. Again, thank you for continuing to make Naval Medical Center Portsmouth the “First and Finest”.
Disclaimer: Please note that information regarding the appropriate diagnosis, management, and disposition of COVID-19 Persons Under Investigation (PUI) or positive patients is changing rapidly. This document is meant to serve as a guideline but may inevitably change as new research or command decisions come to light. Lastly, this guide was designed to be an adjunct to assist with patient management but is in no way a substitute for individual clinical judgment and medical decision making.
B. Basic Science/Epidemiology
1. Biology
Novel coronavirus, or SARS-CoV-2, is a non-segmented, positive sense RNA virus that belongs to the larger coronavirus family, of which there are now seven known members. Four of these viruses are responsible for mild respiratory illness including the common cold [229E, NL63, OC43, HKU1] while MERS-CoV and SARS-CoV-1 cause MERS and SARS respectively.
SARS-CoV-2, which causes novel coronavirus 2019 or COVID-19, is most closely associated with SARS-CoV-1, the virus responsible for the SARS epidemic in 2003. A significant relation between the two viruses is the mechanism by which they enter host cells: the ACE2 receptor, a receptor that has been shown to be present on type II pneumocytes, intestinal epithelia, and nasal mucosa in addition to many other locations.
2. Pathophysiology

1. Hypoxemic respiratory failure
a. Pneumocytes have been shown undergo cytopathic effect, indicating direct viral damage rather than damage secondary to inflammation.
b. COVID-19 has also been shown to reduce surfactant levels, leading to alveolar collapse, atelectasis, and de-recruitment.
c. Likely mechanism of lung injury is “diffuse alveolar damage” or Acute Respiratory Distress Syndrome (ARDS), which has led to the adoption of many principles of ARDS management for COVID-19 patients.
2. Cytokine Storm
a. Around day 7-10 of illness patients can acutely worsen which can manifest as recalcitrant fever, cytopenias, elevated liver associated enzymes, multi-organ system failure, elevated ferritin levels, and disseminated intravascular coagulation.
b. This has been shown to likely be related to immunological hyperactivation triggered by the virus or its associated immune response, similar to hemophagocytic lymphohistiocytosis (HLH) or CAR-T cell cytokine release syndrome but appears to be distinct from these conditions.
3. Disseminated Intravascular Coagulation
a. Later in the disease course, patients can present with signs of disseminated intravascular coagulation (DIC) with rising d-dimer correlated to poorer prognosis.
b. Etiology could be secondary to HLH-like immunologic activation and associated up-regulation of fibrinogen versus direct binding of the virus to ACE2 receptors on endothelial cells.
4. Pro-thrombotic and inflammatory pathophysiology and consequences
a. Venous thromboembolism (VTE), including extensive deep vein thrombosis (DVT) and pulmonary embolism (PE), is very common in acutely ill patients with COVID-19, seen in up to one-third of patients in the intensive care unit (ICU), even when prophylactic anticoagulation is used.
b. This state has been termed thromboinflammation or COVID-19-associated coagulopathy (CAC) by some experts. It appears to be distinct from disseminated intravascular coagulation (DIC), though DIC has been reported in severely affected patients (as discussed above).
c. There are also reports of arterial thrombosis, including in the central nervous system (CNS). The largest study, which included 3334 individuals (829 ICU and 2505 non-ICU) reported stroke in 1.6 percent and myocardial infarction in 8.9 percent.
3. Transmission
COVID-19 has been shown to have various modes of transmission that impact how we appropriately care for these patients as well as the healthcare staff to ensure safety and limit spread of infection.
1. Large Droplet Transmission
a. A primary mode of transmission was found in large droplet transmission, which is typical for respiratory viruses such as influenza. Most societies recommend that risk is greatest within 6 feet of an actively infected patient.
b. Risk is mitigated to an acceptable degree by the patient and provider wearing a standard surgical mask.
2. Airborne Transmission
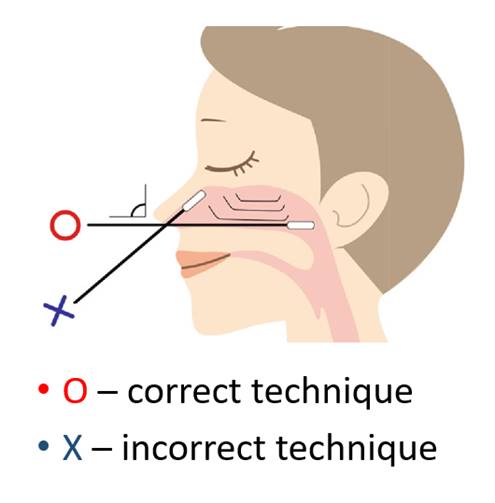
a. There is increasing evidence that COVID-19 can also be transmitted via an airborne route, thus implying the need for a provider to wear a fitted N95 mask.
b. There have been recent studies to suggest that COVID-19 can persist in aerosols for hours.
c. Most transmission is still believed to occur by droplet rather than aerosol transmission, though certain medical procedures may increase the risk of aerosolization.
d. Negative pressure isolation is ideal; however, availability and initial risk assessment will determine which patients are placed in isolation
3. Contact Transmission
a. COVID-19 has been shown to persist on certain fomites for up to 4 days, lending to a possible risk for inoculation through direct contact.
b. When a patient coughs, droplets deposit on fomites creating a thin film. A second, uninfected person can come in contact with the fomite, touch mucosal membranes and become inoculated.
c. This can be mitigated with regular deep cleaning of rooms during turnover, thorough and frequent hand washing, and avoidance of facial touching.
The Basic Reproduction Number, Rø, is an epidemiologic term that can be thought of as the expected number of cases directly generated by one case in a population where all individuals are susceptible to infection. If Rø is < 1, the disease will eventually burn out. If Rø is > 1, the disease will increasingly infect hosts in an exponential fashion. Current Rø estimates for COVID-19 are approximately 2.5-2.9.
Importantly, Rø is a reflection of transmissibility, contact between susceptible and infected individuals (human behavior), and duration of infectiousness. Public health measures such as physical distancing and closing public businesses have had significant impact on the effective reproduction number over time, Rt or Re. Additionally, there is recent evidence to suggest that R may vary between different individuals depending on things like their contact rate with others and viral load. An asymptomatic patient with a high-viral load, or high contact rate, may infect many more people (super-spreader) than a similar patient with lower viral load or contact rate.
C. Personal Protective Equipment
Protecting yourself, as a healthcare worker (HCW), before entering the room of a patient suspected of having COVID-19 with the proper equipment is paramount to limiting the spread of infection to yourself and other coworkers. This could have significant consequences regarding staff shortages for our hospital as well as putting the community at risk. Even more important is learning the correct protocol for donning and doffing this equipment.
Important for preventing transmission of SARS-CoV-2 in the healthcare settings is having at least two layers of protection for all contacts (non-COVID-19 patient to HCW, HCW to HCW, etc.). One layer is your own mask. The second can be a mask on the patient or eye protection on you (or both).
This video from the DoD CPG Guideline reviews procedures:
https://www.youtube.com/watch?v=bG6zISnenPg
1. Donning
a. The correct order for donning personal protective equipment (PPE) prior to entering the room of a patient suspected of having COVID-19 is GOWN, MASK, GOGGLES/FACE SHIELD, THEN GLOVES.
2. Doffing
a. Doffing PPE is often considered the more challenging step as well as the most important to ensure mitigation of potential spread.
b. Prior to beginning the doffing process, first apply hand sanitizer from inside the room to your gloves.
c. Carefully remove gown by pulling the chest area forward, ensuring to keep the gown forward and have the waste bin open.
d. Carefully roll the gown inside out over the gloves while simultaneous removing the gloves.
e. Discard bundle of rolled gown and gloves into waste bin.
f. Clean your hands with soap and water and re-don gloves. Carefully remove your eyewear touching only the rear-most part of the ear pieces and wipe them down thoroughly with approved sanitizer wipes .
g. Only once a-f is complete, can you leave the room into the ante room.
h. Once in the ante room, follow standard procedure for washing hands
i. While leaning over the waste bin the ante room, carefully remove the straps from the N95 mask and let the mask fall into the waste bin.
j. NOTE: If conserving goggles and/or N95 mask please follow ward instructions for proper conservation.
D. Clinical Features at Presentation
The clinical illness script for COVID-19 is constantly changing as more cases are discovered. However, many patients present with lower respiratory symptoms such as cough or dyspnea, fever, upper respiratory symptoms, and/or gastrointestinal symptoms. Incubation period is a median of 4 days with a range of 14 days. Common presenting symptoms (with percent displaying this symptom at presentation include:

1. Fever
a. Data has shown that fever is present in about 50% of patients at the time of hospital admission, signifying that absence of fever does not exclude COVID-19.
2. Gastrointestinal Symptoms
a. 10% of patients may present with nausea or diarrhea which precede the onset of respiratory symptoms.
3. “Silent hypoxemia”
a. There is a subset of patients that present with nonspecific symptoms and are found to be hypoxemic without dyspnea.
4. Taste/Smell: About 25% of patients will have disturbance in taste or smell.
E. Additional Resources
Additional resources for more detail (and that are updated routinely) include:
1. The Internet Book of Critical Care (IBCC): A continuously peer reviewed and updated summary of the literature is available from the IBCC at: https://emcrit.org/ibcc/covid19/
2. DoD Clinical Practice Guideline (CPG): The DoD has a published practice guideline for COVID-19 available in the same drive as this document.
3. American College of Physicians Course on COVID-19: The ACP (internal medicine professional society) has a more in-depth course on COVID that is also updated regularly that walks through the basics of coronaviruses up through current treatments and approaches to COVID-19 and provides a large assortment of resources for further information.
4. Infectious Disease Society of America Guidelines
5. National Institute of Health Guidelines
6. Surviving Sepsis COVID-19 Guidelines